Abstract
Background
Emerging evidence suggests that per- and polyfluoroalkyl substances (PFAS) are endocrine disruptors and may contribute to the etiology of diabetes.
Objectives
This study aimed to systematically review the epidemiological evidence on the associations of PFAS with mortality and morbidity of diabetes and to quantitatively evaluate the summary effect estimates of the existing literature.
Methods
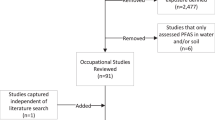
We searched three electronic databases for epidemiological studies concerning PFAS and diabetes published before April 1, 2022. Summary odds ratio (OR), hazard ratio (HR), or β and their 95% confidence intervals (CIs) were respectively calculated to evaluate the association between PFAS and diabetes using random-effects model by the exposure type, and dose-response meta-analyses were also performed when possible. We also assessed the risk of bias of the studies included and the confidence in the body of evidence.
Results
An initial literature search identified 1969 studies, of which 22 studies were eventually included. The meta-analyses indicated that the observed statistically significant PFAS-T2DM associations were consistent in cohort studies, while the associations were almost non-significant in case-control and cross-sectional studies. Dose-response meta-analysis showed a “parabolic-shaped” association between perfluorooctanoate acid (PFOA) exposure and T2DM risk. Available evidence was rated with “low” risk of bias, and the level of evidence for PFAS and incident T2DM was considered “moderate”.
Conclusions
Our findings suggest that PFAS exposure may increase the risk of incident T2DM, and that PFOA may exert non-monotonic dose-response effect on T2DM risk. Considering the widespread exposure, persistence, and potential for adverse health effects of PFAS, further cohort studies with improvements in expanding the sample size, adjusting the covariates, and considering different types of PFAS exposure at various doses, are needed to elucidate the putative causal associations and potential mode of action of different PFAS on diabetes.
Impact Statement
A growing body of evidence suggests that per- and polyfluoroalkyl substances (PFAS) are endocrine disruptors and may contribute to the development of diabetes. However, epidemiological evidence on the associations of PFAS and diabetes is inconsistent. We performed this comprehensive systematic review and meta-analysis to quantitatively synthesize the evidence. The findings of this study suggest that exposure to PFAS may increase diabetes risk among the general population. Reduced exposure to these “forever and everywhere chemicals” may be an important preventative approach to reducing the risk of diabetes across the population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The dataset generated and/or analyzed in the current study can be obtained from the corresponding author on a reasonable request.
References
Calafat AM, Kuklenyik Z, Reidy JA, Caudill SP, Tully JS, Needham LL. Serum concentrations of 11 polyfluoroalkyl compounds in the u.s. population: data from the national health and nutrition examination survey (NHANES). Environ Sci Technol. 2007;41:2237–42.
Sima MW, Jaffé PR. A critical review of modeling Poly- and Perfluoroalkyl Substances (PFAS) in the soil-water environment. Sci Total Environ. 2021;757:143793.
Abbott BD, Wolf CJ, Schmid JE, Das KP, Zehr RD, Helfant L, et al. Perfluorooctanoic acid induced developmental toxicity in the mouse is dependent on expression of peroxisome proliferator activated receptor-alpha. Toxicol Sci. 2007;98:571–81.
Schroeder T, Bond D, Foley J. PFAS soil and groundwater contamination via industrial airborne emission and land deposition in SW Vermont and Eastern New York State, USA. Environ Sci Process Impacts. 2021;23:291–301.
Zeeshan M, Zhang YT, Yu S, Huang WZ, Zhou Y, Vinothkumar R, et al. Exposure to isomers of per- and polyfluoroalkyl substances increases the risk of diabetes and impairs glucose-homeostasis in Chinese adults: Isomers of C8 health project. Chemosphere. 2021;278:130486.
Wang Z, DeWitt JC, Higgins CP, Cousins ITA. Never-Ending Story of Per- and Polyfluoroalkyl Substances (PFASs)? Environ Sci Technol. 2017;51:2508–18.
Steenland K, Fletcher T, Savitz DA. Epidemiologic evidence on the health effects of perfluorooctanoic acid (PFOA). Environ Health Perspect. 2010;118:1100–8.
Vestergren R, Cousins IT. Tracking the pathways of human exposure to perfluorocarboxylates. Environ Sci Technol. 2009;43:5565–75.
Silva JAK, Martin WA, McCray JE. Air-water interfacial adsorption coefficients for PFAS when present as a multi-component mixture. J Contam Hydrol. 2021;236:103731.
Chang ET, Adami HO, Boffetta P, Cole P, Starr TB, Mandel JS. A critical review of perfluorooctanoate and perfluorooctanesulfonate exposure and cancer risk in humans. Crit Rev Toxicol. 2014;44:1–81.
Chang ET, Adami HO, Boffetta P, Wedner HJ, Mandel JS. A critical review of perfluorooctanoate and perfluorooctanesulfonate exposure and immunological health conditions in humans. Crit Rev Toxicol. 2016;46:279–331.
Bach C, Dauchy X, Boiteux V, Colin A, Hemard J, Sagres V, et al. The impact of two fluoropolymer manufacturing facilities on downstream contamination of a river and drinking water resources with per- and polyfluoroalkyl substances. Environ Sci Pollut Res Int. 2017;24:4916–25.
Conway BN, Badders AN, Costacou T, Arthur JM, Innes KE. Perfluoroalkyl substances and kidney function in chronic kidney disease, anemia, and diabetes. Diabetes Metab Syndr Obes. 2018;11:707–16.
Stratakis N, Jin DVC, Margetaki R, Valvi K, Siskos D AP, et al Prenatal Exposure to Perfluoroalkyl Substances Associated With Increased Susceptibility to Liver Injury in Children. Hepatology. 2020;72:1758–70.
Kim MJ, Moon S, Oh BC, Jung D, Ji K, Choi K, et al. Association between perfluoroalkyl substances exposure and thyroid function in adults: A meta-analysis. PLoS One. 2018;13:e0197244.
Kharroubi AT, Darwish HM. Diabetes mellitus: The epidemic of the century. World J Diabetes. 2015;6:850–67.
Boyle JP, Honeycutt AA, Narayan KM, Hoerger TJ, Geiss LS, Chen H, et al. Projection of diabetes burden through 2050: impact of changing demography and disease prevalence in the U.S. Diabetes Care. 2001;24:1936–40.
Liu H, Duan JQ, Ren XM, Li XL, Chen J, Li P, et al. [Changes of Gene Expression Profile in Cardiac Mesenchymal Cells in Patients with Type 2 Diabetes Mellitus and Screening of Their Related Environmental Chemicals]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2020;42:37–46.
Mancini FR, Rajaobelina K, Praud D, Dow C, Antignac JP, Kvaskoff M, et al. Nonlinear associations between dietary exposures to perfluorooctanoic acid (PFOA) or perfluorooctane sulfonate (PFOS) and type 2 diabetes risk in women: Findings from the E3N cohort study. Int J Hyg Environ Health. 2018;221:1054–60.
Pfohl M, Marques E, Auclair A, Barlock B, Jamwal R, Goedken M, et al. An ‘Omics Approach to Unraveling the Paradoxical Effect of Diet on Perfluorooctanesulfonic Acid (PFOS) and Perfluorononanoic Acid (PFNA)-Induced Hepatic Steatosis. Toxicol Sci. 2021;180:277–94.
Wielsøe M, Long M, Ghisari M, Bonefeld-Jørgensen EC. Perfluoroalkylated substances (PFAS) affect oxidative stress biomarkers in vitro. Chemosphere. 2015;129:239–45.
Donat-Vargas C, Bergdahl IA, Tornevi A, Wennberg M, Sommar J, Kiviranta H, et al. Perfluoroalkyl substances and risk of type II diabetes: A prospective nested case-control study. Environ Int. 2019;123:390–8.
He X, Liu Y, Xu B, Gu L, Tang W. PFOA is associated with diabetes and metabolic alteration in US men: National Health and Nutrition Examination Survey 2003–12. Sci Total Environ. 2018;625:566–74.
MacNeil J, Steenland NK, Shankar A, Ducatman A. A cross-sectional analysis of type II diabetes in a community with exposure to perfluorooctanoic acid (PFOA). Environ Res. 2009;109:997–1003.
McGlinchey A, Sinioja T, Lamichhane S, Sen P, Bodin J, Siljander H, et al. Prenatal exposure to perfluoroalkyl substances modulates neonatal serum phospholipids, increasing risk of type 1 diabetes. Environ Int. 2020;143:105935.
Su TC, Kuo CC, Hwang JJ, Lien GW, Chen MF, Chen PC. Serum perfluorinated chemicals, glucose homeostasis and the risk of diabetes in working-aged Taiwanese adults. Environ Int. 2016;88:15–22.
Taylor KW, Novak RF, Anderson HA, Birnbaum LS, Blystone C, Devito M, et al. Evaluation of the association between persistent organic pollutants (POPs) and diabetes in epidemiological studies: a national toxicology program workshop review. Environ Health Perspect. 2013;121:774–83.
Qi W, Clark JM, Timme-Laragy AR, Park Y. Per- and Polyfluoroalkyl Substances and Obesity, Type 2 Diabetes and Non-alcoholic Fatty Liver Disease: A Review of Epidemiologic Findings. Toxicol Environ Chem. 2020;102:1–36.
Predieri B, Bruzzi P, Bigi E, Ciancia S, Madeo SF, Lucaccioni L, et al. Endocrine Disrupting Chemicals and Type 1 Diabetes. Int J Mol Sci. 2020;21:2937.
Howard SG. Exposure to environmental chemicals and type 1 diabetes: an update. J Epidemiol Community Health. 2019;73:483–8.
Bodin J, Stene LC, Nygaard UC. Can exposure to environmental chemicals increase the risk of diabetes type 1 development? Biomed Res Int. 2015;2015:208947.
Lind PM, Lind L. Endocrine-disrupting chemicals and risk of diabetes: an evidence-based review. Diabetologia. 2018;61:1495–502.
Gao X, Ni W, Zhu S, Wu Y, Cui Y, Ma J, et al. Per- and polyfluoroalkyl substances exposure during pregnancy and adverse pregnancy and birth outcomes: A systematic review and meta-analysis. Environ Res. 2021;201:111632.
Wang J, Zhang J, Fan Y, Li Z, Tao C, Yan W, et al. Association between per- and polyfluoroalkyl substances and risk of gestational diabetes mellitus. Int J Hyg Environ health. 2022;240:113904.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Rooney AA, Boyles AL, Wolfe MS, Bucher JR, Thayer KA. Systematic review and evidence integration for literature-based environmental health science assessments. Environ Health Perspect. 2014;122:711–8.
Morgan RL, Beverly B, Ghersi D, Schünemann HJ, Rooney AA, Whaley P, et al. GRADE guidelines for environmental and occupational health: A new series of articles in Environment. Int Environ Int. 2019;128:11–12.
Cano-Sancho G, Ploteau S, Matta K, Adoamnei E, Louis GB, Mendiola J, et al. Human epidemiological evidence about the associations between exposure to organochlorine chemicals and endometriosis: Systematic review and meta-analysis. Environ Int. 2019;123:209–23.
Lai KY, Sarkar C, Ni MY, Cheung LWT, Gallacher J, Webster C. Exposure to light at night (LAN) and risk of breast cancer: A systematic review and meta-analysis. Sci total Environ. 2021;762:143159.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Raffetti E, Donat-Vargas C, Mentasti S, Chinotti A, Donato F. Association between exposure to polychlorinated biphenyls and risk of hypertension: A systematic review and meta-analysis. Chemosphere. 2020;255:126984.
Hu XF, Lowe M, Chan HM. Mercury exposure, cardiovascular disease, and mortality: A systematic review and dose-response meta-analysis. Environ Res. 2021;193:110538.
Bartell SM, Vieira VM. Critical review on PFOA, kidney cancer, and testicular cancer. J Air Waste Manag Assoc. 2021;71:663–79.
Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. 1992;135:1301–9.
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol. 2012;175:66–73.
Crippa A, Discacciati A, Bottai M, Spiegelman D, Orsini N. One-stage dose-response meta-analysis for aggregated data. Stat Methods Med Res. 2019;28:1579–96.
Filippini T, Torres D, Lopes C, Carvalho C, Moreira P, Naska A, et al. Cadmium exposure and risk of breast cancer: A dose-response meta-analysis of cohort studies. Environ Int. 2020;142:105879.
Christensen KY, Raymond M, Thompson BA, Anderson HA. Perfluoroalkyl substances in older male anglers in Wisconsin. Environ Int. 2016;91:312–8.
Park SK, Wang X, Ding N, Karvonen-Gutierrez CA, Calafat AM, Herman WH, et al. Per- and polyfluoroalkyl substances and incident diabetes in midlife women: the Study of Women’s Health Across the Nation (SWAN). Diabetologia. 2022. https://doi.org/10.1007/s00125-022-05695-5.
Boonhat H, Lin RT. Association between leukemia incidence and mortality and residential petrochemical exposure: A systematic review and meta-analysis. Environ Int. 2020;145:106090.
Eze IC, Hemkens LG, Bucher HC, Hoffmann B, Schindler C, Künzli N, et al. Association between ambient air pollution and diabetes mellitus in Europe and North America: systematic review and meta-analysis. Environ Health Perspect. 2015;123:381–9.
Cardenas A, Hivert MF, Gold DR, Hauser R, Kleinman KP, Lin PD, et al. Associations of Perfluoroalkyl and Polyfluoroalkyl Substances With Incident Diabetes and Microvascular Disease. Diabetes Care. 2019;42:1824–32.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Fan SJ, Heinrich J, Bloom MS, Zhao TY, Shi TX, Feng WR, et al. Ambient air pollution and depression: A systematic review with meta-analysis up to 2019. Sci Total Environ. 2020;701:134721.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315:629–34.
Charles D, Berg V, Nøst TH, Huber S, Sandanger TM, Rylander C. Pre- and post-diagnostic blood profiles of perfluoroalkyl acids in type 2 diabetes mellitus cases and controls. Environ Int. 2020;145:106095.
Conway B, Innes KE, Long D. Perfluoroalkyl substances and beta cell deficient diabetes. J Diabetes Complications. 2016;30:993–8.
Duan Y, Sun H, Yao Y, Li Y, Meng Y, Lu Y, et al. Serum concentrations of per-/polyfluoroalkyl substances and risk of type 2 diabetes: A case-control study. Sci Total Environ. 2021;787:147476.
Han X, Meng L, Zhang G, Li Y, Shi Y, Zhang Q, et al. Exposure to novel and legacy per- and polyfluoroalkyl substances (PFASs) and associations with type 2 diabetes: A case-control study in East China. Environ Int. 2021;156:106637.
Sun Q, Zong G, Valvi D, Nielsen F, Coull B, Grandjean P. Plasma Concentrations of Perfluoroalkyl Substances and Risk of Type 2 Diabetes: A Prospective Investigation among U.S. Women. Environ Health Perspect. 2018;126:037001.
Fleisch AF, Rifas-Shiman SL, Mora AM, Calafat AM, Ye X, Luttmann-Gibson H, et al. Early-Life Exposure to Perfluoroalkyl Substances and Childhood Metabolic Function. Environ Health Perspect. 2017;125:481–7.
Kim JH, Park HY, Jeon JD, Kho Y, Kim SK, Park MS, et al. The modifying effect of vitamin C on the association between perfluorinated compounds and insulin resistance in the Korean elderly: a double-blind, randomized, placebo-controlled crossover trial. Eur J Nutr. 2016;55:1011–20.
Karnes C, Winquist A, Steenland K. Incidence of type II diabetes in a cohort with substantial exposure to perfluorooctanoic acid. Environ Res. 2014;128:78–83.
Steenland K, Zhao L, Winquist A, Parks C. Ulcerative colitis and perfluorooctanoic acid (PFOA) in a highly exposed population of community residents and workers in the mid-Ohio valley. Environ Health Perspect. 2013;121:900–5.
Lind L, Zethelius B, Salihovic S, van Bavel B, Lind PM. Circulating levels of perfluoroalkyl substances and prevalent diabetes in the elderly. Diabetologia. 2014;57:473–9.
Zhang YT, Zeeshan M, Su F, Qian ZM, Dee Geiger S, Edward, et al. Associations between both legacy and alternative per- and polyfluoroalkyl substances and glucose-homeostasis: The Isomers of C8 health project in China. Environ Int. 2022;158:106913.
Cardenas A, Gold DR, Hauser R, Kleinman KP, Hivert MF, Calafat AM, et al. Plasma Concentrations of Per- and Polyfluoroalkyl Substances at Baseline and Associations with Glycemic Indicators and Diabetes Incidence among High-Risk Adults in the Diabetes Prevention Program Trial. Environ Health Perspect. 2017;125:107001.
Lin CY, Chen PC, Lin YC, Lin LY. Association among serum perfluoroalkyl chemicals, glucose homeostasis, and metabolic syndrome in adolescents and adults. Diabetes Care. 2009;32:702–7.
Nelson JW, Hatch EE, Webster TF. Exposure to polyfluoroalkyl chemicals and cholesterol, body weight, and insulin resistance in the general U.S. population. Environ Health Perspect. 2010;118:197–202.
Steenland K, Woskie S. Cohort mortality study of workers exposed to perfluorooctanoic acid. Am J Epidemiol. 2012;176:909–17.
Gilliland FD, Mandel JS. Mortality among employees of a perfluorooctanoic acid production plant. J Occup Med. 1993;35:950–4.
Leonard RC, Kreckmann KH, Sakr CJ, Symons JM. Retrospective cohort mortality study of workers in a polymer production plant including a reference population of regional workers. Ann Epidemiol. 2008;18:15–22.
Raleigh KK, Alexander BH, Olsen GW, Ramachandran G, Morey SZ, Church TR, et al. Mortality and cancer incidence in ammonium perfluorooctanoate production workers. Occup Environ Med. 2014;71:500–6.
Mastrantonio M, Bai E, Uccelli R, Cordiano V, Screpanti A, Crosignani P. Drinking water contamination from perfluoroalkyl substances (PFAS): an ecological mortality study in the Veneto Region, Italy. Eur J Public Health. 2018;28:180–5.
Lundin JI, Alexander BH, Olsen GW, Church TR. Ammonium perfluorooctanoate production and occupational mortality. Epidemiology. 2009;20:921–8.
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pr. 2019;157:107843.
Hines EP, White SS, Stanko JP, Gibbs-Flournoy EA, Lau C, Fenton SE. Phenotypic dichotomy following developmental exposure to perfluorooctanoic acid (PFOA) in female CD-1 mice: Low doses induce elevated serum leptin and insulin, and overweight in mid-life. Mol Cell Endocrinol. 2009;304:97–105.
Lv Z, Li G, Li Y, Ying C, Chen J, Chen T, et al. Glucose and lipid homeostasis in adult rat is impaired by early-life exposure to perfluorooctane sulfonate. Environ Toxicol. 2013;28:532–42.
Wan HT, Zhao YG, Leung PY, Wong CK. Perinatal exposure to perfluorooctane sulfonate affects glucose metabolism in adult offspring. PLoS One. 2014;9:e87137.
Behr AC, Plinsch C, Braeuning A, Buhrke T. Activation of human nuclear receptors by perfluoroalkylated substances (PFAS). Toxicol Vitr. 2020;62:104700.
Ishibashi H, Hirano M, Kim EY, Iwata H. In Vitro and In Silico Evaluations of Binding Affinities of Perfluoroalkyl Substances to Baikal Seal and Human Peroxisome Proliferator-Activated Receptor α. Environ Sci Technol. 2019;53:2181–8.
De Silva AO, Armitage JM, Bruton TA, Dassuncao C, Heiger-Bernays W, Hu XC, et al. PFAS Exposure Pathways for Humans and Wildlife: A Synthesis of Current Knowledge and Key Gaps in Understanding. Environ Toxicol Chem. 2021;40:631–57.
Pedersen KE, Letcher RJ, Sonne C, Dietz R, Styrishave B. Per- and polyfluoroalkyl substances (PFASs) - New endocrine disruptors in polar bears (Ursus maritimus)? Environ Int. 2016;96:180–9.
Takacs ML, Abbott BD. Activation of mouse and human peroxisome proliferator-activated receptors (alpha, beta/delta, gamma) by perfluorooctanoic acid and perfluorooctane sulfonate. Toxicol Sci. 2007;95:108–17.
Botta M, Audano M, Sahebkar A, Sirtori CR, Mitro N, Ruscica M. PPAR Agonists and Metabolic Syndrome: An Established Role? Int J Mol Sci. 2018;19:1197.
Wolf CJ, Schmid JE, Lau C, Abbott BD. Activation of mouse and human peroxisome proliferator-activated receptor-alpha (PPARα) by perfluoroalkyl acids (PFAAs): further investigation of C4-C12 compounds. Reprod Toxicol. 2012;33:546–51.
Gurnell M. ‘Striking the Right Balance’ in Targeting PPARgamma in the Metabolic Syndrome: Novel Insights from Human Genetic Studies. PPAR Res. 2007;2007:83593.
Yu XH, Zheng XL, Tang CK. Peroxisome Proliferator-Activated Receptor α in Lipid Metabolism and Atherosclerosis. Adv Clin Chem. 2015;71:171–203.
Park SK, Ding N, Han D. Perfluoroalkyl substances and cognitive function in older adults: Should we consider non-monotonic dose-responses and chronic kidney disease? Environ Res. 2021;192:110346.
Dhingra R, Winquist A, Darrow LA, Klein M, Steenland KA. Study of Reverse Causation: Examining the Associations of Perfluorooctanoic Acid Serum Levels with Two Outcomes. Environ Health Perspect. 2017;125:416–21.
Jain RB, Ducatman A. Perfluoroalkyl substances follow inverted U-shaped distributions across various stages of glomerular function: Implications for future research. Environ Res. 2019;169:476–82.
Funding
This study was supported by Key Projects of Natural Science Research of Anhui Provincial Department of Education (KJ2020A0163) and National Natural Science Foundation of China (82070986).
Author information
Authors and Affiliations
Contributions
CYH and ZXJ conceived of and coordinated the study. SYG, JCQ, KXW, ZLL, KJW and YNC searched the literature, extracted and analyzed the data, and drafted the manuscript. SYG, JCQ, KXW, ZLL, KJW, YNC, and CYH interpreted the results and drafted and revised the manuscript. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gui, SY., Qiao, JC., Xu, KX. et al. Association between per- and polyfluoroalkyl substances exposure and risk of diabetes: a systematic review and meta-analysis. J Expo Sci Environ Epidemiol 33, 40–55 (2023). https://doi.org/10.1038/s41370-022-00464-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-022-00464-3
Keywords
This article is cited by
-
Associations of per- and polyfluoroalkyl substances (PFAS) and their mixture with risk of rheumatoid arthritis in the U.S. adult population
Environmental Health (2024)
-
Perfluorooctane sulfonic acid exposure and diabetes: a cross-sectional analysis of American adults and in vitro experiments
Environmental Sciences Europe (2023)
-
PFAS concentrations in early and mid-pregnancy and risk of gestational diabetes mellitus in a nested case-control study within the ethnically and racially diverse PETALS cohort
BMC Pregnancy and Childbirth (2023)